Varicose veins of the lower extremities or varicose veins of the lower extremities is a pathological condition associated with the expansion of the superficial saphenous veins, valve failure in them and progressive venous congestion in the lower extremities
It is statistically known that the fair half of the population is more susceptible to vein diseases (varicose veins of the lower extremities). According to various authors, the incidence among the female half is from 40 to 89%, among men – from 32 to 66%. Yes, these ratings mention all cases of varicose veins, including clinically insignificant ones, for example, spider veins, but nevertheless, half of these patients, in addition to aesthetic discomfort, experience certain complaints associated with progressive venous insufficiency.
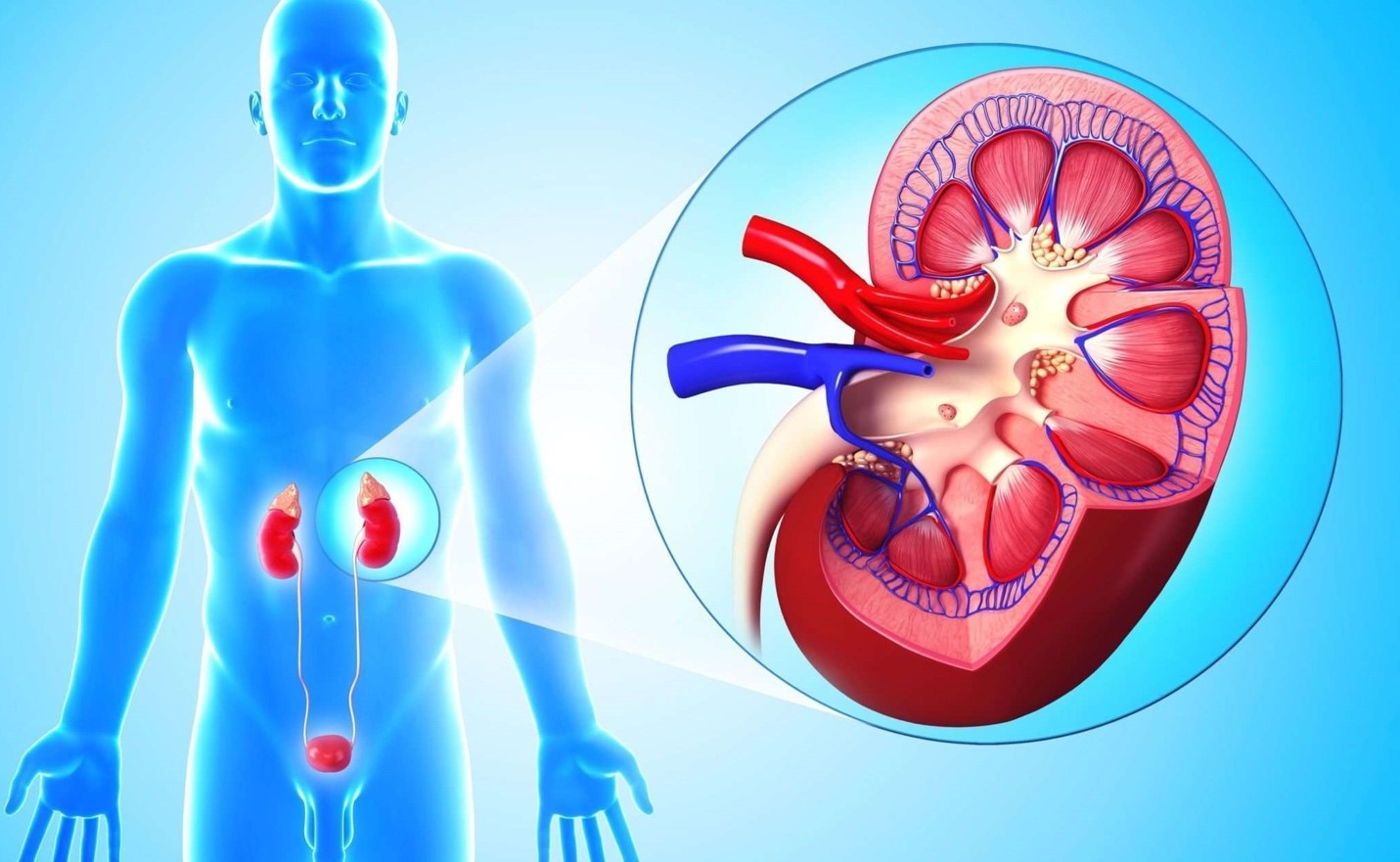
A little about the anatomy of the veins of the lower extremities. Veins of the legs are represented by three main types:
Basin of the main saphenous veins (great and small saphenous veins). The above veins collect venous blood from the surface tissues (skin, subcutaneous tissue) of the lower extremities. These veins are most often affected by varicose veins. Due to the deep bedding of the main saphenous veins on the thigh and, sometimes, on the lower leg, we do not see changes in the highways, but we notice only altered convoluted wreaths at the level of the skin of the lower leg. It should be borne in mind that with a significant, large varicose vein on the lower leg, there are also changes on the thigh, in the main vein, it is simply not visible with the eye.
Deep vein pool. These veins are located deep in the thickness of muscles and other tissues. We do not see these veins, and it is worth knowing that deep veins are not affected by varicose veins, and changes with valves in them occur only after previous diseases (deep vein thrombosis, serious injuries, etc.)
A pool of vein perforators (or communicators). These veins connect the deep and superficial veins. Unlike the saphenous and deep veins, which run from the foot to the heart (bottom to top), perforating veins extend from the skin level into the tissues.
A few words about the classification of varicose veins.
The most complete assessment of the condition and severity of the disease is provided by the modern CEAP classification, it is convenient, but difficult to use and is understandable only for specialists dealing with altered veins every day. Let’s dwell on one of the classifications in accordance with the diameter of the veins:
Spider veins or telangiectasias are small (up to 1 mm) intradermal veins visible to the eye. In addition to aesthetic discomfort, as a rule, they do not cause any significant clinical manifestations.
Reticular or intradermal varicose veins – changed veins, with a diameter of 1 to 3 mm. As well as the previous group, it causes, to a greater extent, aesthetic discomfort than significant clinical manifestations.
Segmental varicose veins – altered, convoluted veins with a diameter of more than 3 mm. As a rule, they originate from the main vein (large or small saphenous vein), perforating vein of the thigh or lower leg. If you have these veins, you should definitely see a doctor.
Changes in the basin of the main saphenous veins (large or small saphenous veins). Require compulsory observation and treatment by a phlebologist or angiosurgeon (vascular surgeon).
Changes in the pool of perforating veins. The assessment of the degree of changes is carried out by a specialist doctor and appropriate therapy is prescribed.
What contributes to varicose veins?
The most reliable reasons include:
Genetic predisposition, i.e. the risk of developing this disease is higher in people whose family has relatives with varicose veins.
Increased body weight. I would like to note that this point is important not only for the development of varicose veins, but also for diabetes mellitus, hypertension and other serious diseases.
Static work (work with prolonged sitting or standing). You should be aware that, unlike arteries, where blood is ejected under high pressure from the heart, blood flows through the veins, to a greater extent, due to external factors: contraction of the leg muscles, compression of the plantar venous arch during walking and strengthening and increasing the depth of breathing during physical activity, which also promotes venous flow.
Injury of a limb with direct damage to veins or large muscles or bones.
The habit of sitting cross-legged. In this case, there is a mechanical compression of the vein and the formation of stagnant phenomena in it.
There are also other reasons.
I would like to add about additional risk factors for varicose veins in pregnant girls. Many who are already familiar with this disease or have heard about it from relatives or friends note that varicose veins appeared during pregnancy and childbirth.
Why is this happening?
There are several provoking factors of varicose veins, not previously mentioned, which are directly related to pregnancy:
Changes in the hormonal background: an increase in the level of progesterone helps to relax the muscle layer of the vein, its overstretching and subsequent, possible, varicose transformation.
An increase in the size of the uterus. In this case, mechanical compression of the main venous collector of the lower half of the body – the inferior vena cava occurs. That is why it is better for pregnant women to sleep on their left side and at least sometimes they are in the kitty pose (standing on all fours) to reduce pressure on the uterus and improve venous outflow.
An increase in the amount of circulating blood, because during pregnancy, the mother’s body supplies blood not only to its own, but also to the baby’s body, which also contributes to an increase in the load on the vessels, including the veins of the legs.
Manifestations of varicose veins and classic complaints:
visible, altered veins
heaviness, fatigue, swelling in the legs, worse in the evening or night
burning sensation along the changed veins
night cramps
In advanced cases, it is also possible:
darkening, induration, itching of the skin, more often in the lower third of the lower leg
the formation of a trophic ulcer
the formation of a dense painful cord, redness along the vein.
The last two points refer to the most significant complications of varicose veins. I would like to pay special attention to the fact that varicose veins are not only a cosmetic problem, but sometimes cause such formidable complications as thrombophlebitis, pulmonary embolism (in this case, a thrombus breaks off from a vein and spreads through the blood stream from where it enters the lungs). Only 25% of patients with varicose veins meet with these complications, but you must agree that it is better to avoid this.
If you or your loved ones have varicose veins, a disease that can lead to serious complications, we strongly recommend visiting a phlebologist (angiosurgeon, vascular surgeon). Within the framework of our center, the whole range of phlebological services is possible (from conservative to surgical treatment).
Diagnostics
It should be noted that, in addition to visual examination, a modern ultrasound examination (duplex, triplex angioscanning of the veins of the lower extremities) is a mandatory standard for diagnostics. Based on the examination and ultrasound results, a comprehensive picture of the condition of the veins and treatment tactics in the presence of changes is compiled.
I would also like to mention the patients at special risk (the presence of varicose veins and identified or suspected thrombophilia). Thrombophilia is a group of congenital or acquired diseases that contribute to increased blood clotting. With thrombophilia, the risk of thrombophlebitis increases several times (in some conditions, tens of times), and in the presence of varicose veins, the situation is even more aggravated.
Even if you have never had thrombophlebitis, and, at the moment, do not have varicose veins, but close female relatives or you have had episodes of miscarriage (another marker of possible thrombophilia), you should definitely seek the advice of an angiosurgeon, as well as be sure to be observed during pregnancy by both a gynecologist and an angiosurgeon.
What are the main recommendations for girls or men who have come across varicose veins in one way or another or want to prevent it:
Avoid static loads as much as possible. Even if your job involves sitting or standing for a long time and you cannot change it. Walk more often, make rolling movements from heel to toe under the table; do dynamic sports: running, walking, swimming, cycling.
Avoid exposure to heat (sauna, steam room, hot shower). On the contrary, a dosed contrast shower (alternating warm and cool water on the lower leg area) has a positive effect on venous circulation
Do not wear high-heeled shoes for a long time or without a heel at all, with flat soles.
After static loads, you should give the legs an elevated position – lie down, and put a blanket, pillow or roller under the leg end to enhance venous outflow from the legs.
At the first manifestations of varicose veins, be sure to consult a specialist.
Treatment methods for varicose veins
Even in the absence of varicose veins, we often meet people with the so-called syndrome of heavy legs (a clinical picture of heaviness, fatigue, swelling of the legs). Pregnant girls, starting from the second trimester of pregnancy, experience the above complaints. There are effective ways to help, including wearing compression hosiery (stockings, tights, pantyhose for pregnant women).
By default, all girls can wear compression class 1 (preventive) stockings and believe me, your legs will definitely say “thank you”. But not everyone and not always have enough grade 1, so a more complete treatment can be recommended only by a specialist in this area.
The recommended period of wearing knitwear for girls without varicose veins is from the 2nd trimester to 2 months after childbirth. In the presence of varicose veins, wearing compression hosiery is constant during the daytime, you can take it off at night. Wear jersey – until the period of radical elimination of varicose veins (i.e., until the operation is performed).
Among other options for conservative treatment, one can note the use of phlebotonics (drugs that increase the tone of the veins and reduce venous congestion), but again, not all drugs are indicated for pregnant women, and only a doctor will give more accurate recommendations.
Ointments, gels … one of the favorite groups of medicines for our Russian patients. It is worth noting a large selection of medicines for the local treatment of varicose veins, but also, I would like to note that the effectiveness of ointments for the treatment of varicose veins is far from the highest.
With regard to surgical treatment – in the presence of changes in the main veins, visually altered veins, the clinical picture of congestive venous insufficiency, surgical treatment is indicated (only after consultation with a specialist).
During pregnancy, a possible operation is postponed until the postpartum period, and during pregnancy the maximum possible prevention is carried out (among which the leading role belongs to the wearing of medical compression underwear).
In our center, all options for the provision of modern cosmetic care and minimally invasive surgical surgery for varicose veins are possible:
Endovenous laser obliteration https://en.wikipedia.org/wiki/Endovenous_laser_treatment (coagulation) of the great veins.
Classic combined phlebectomy
Sclerotherapy of telangiectasias and reticular veins
Coagulation with radio telangiectasia.
The decision on the choice of a particular technique is made by the attending physician only after a visual examination and performing duplex angioscanning of the veins of the lower extremities.
And finally, one popular adage: “The best treatment is prevention.” It is better to come to an appointment once and make sure that everything is fine and be calm, or catch the disease in the early stages and prevent it from developing, than to deal with the consequences later.